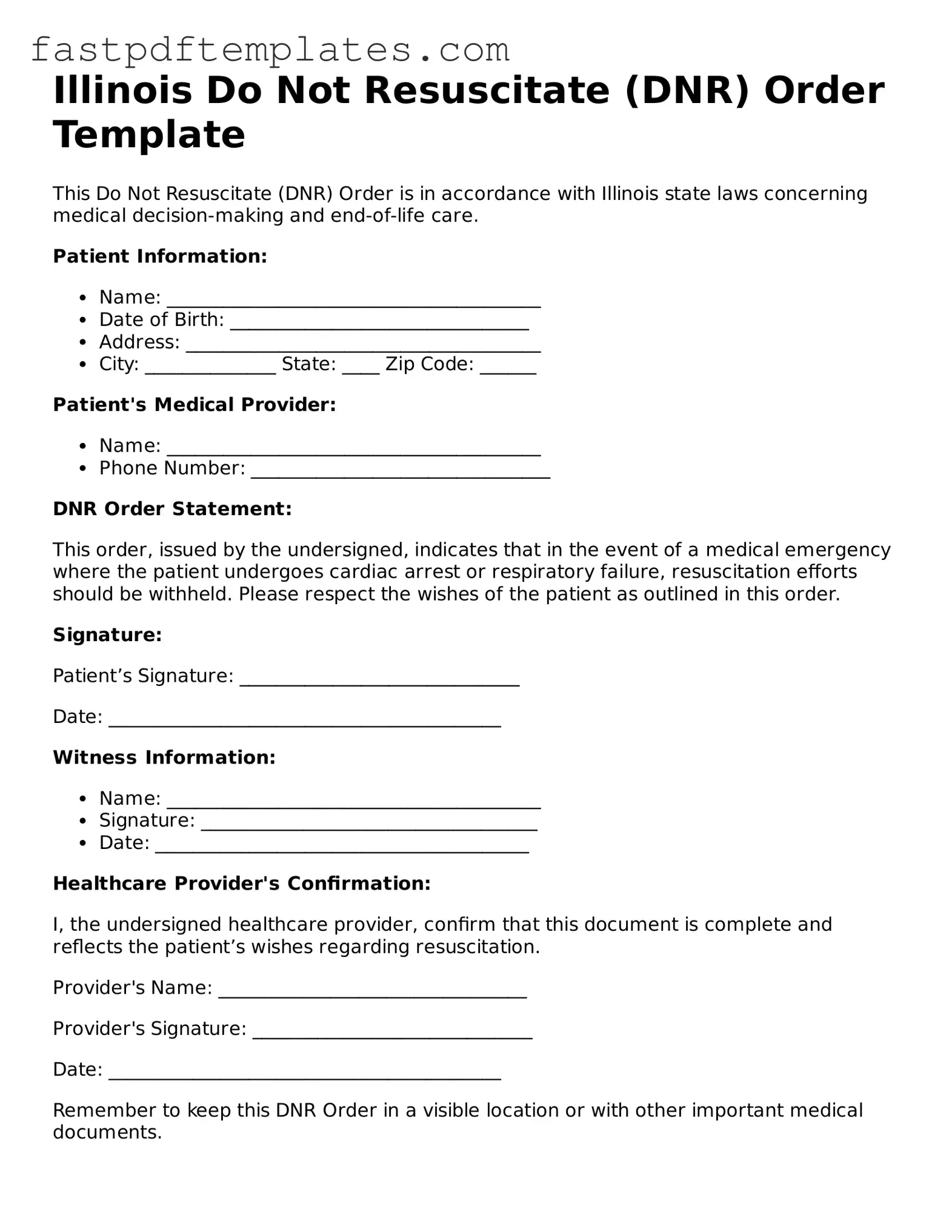
Attorney-Approved Illinois Do Not Resuscitate Order Document
A Do Not Resuscitate (DNR) Order is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. In Illinois, this form provides clarity for healthcare providers and loved ones about a person's preferences when it comes to life-saving interventions. Understanding the DNR Order is essential for anyone considering their end-of-life care options.
Access Document
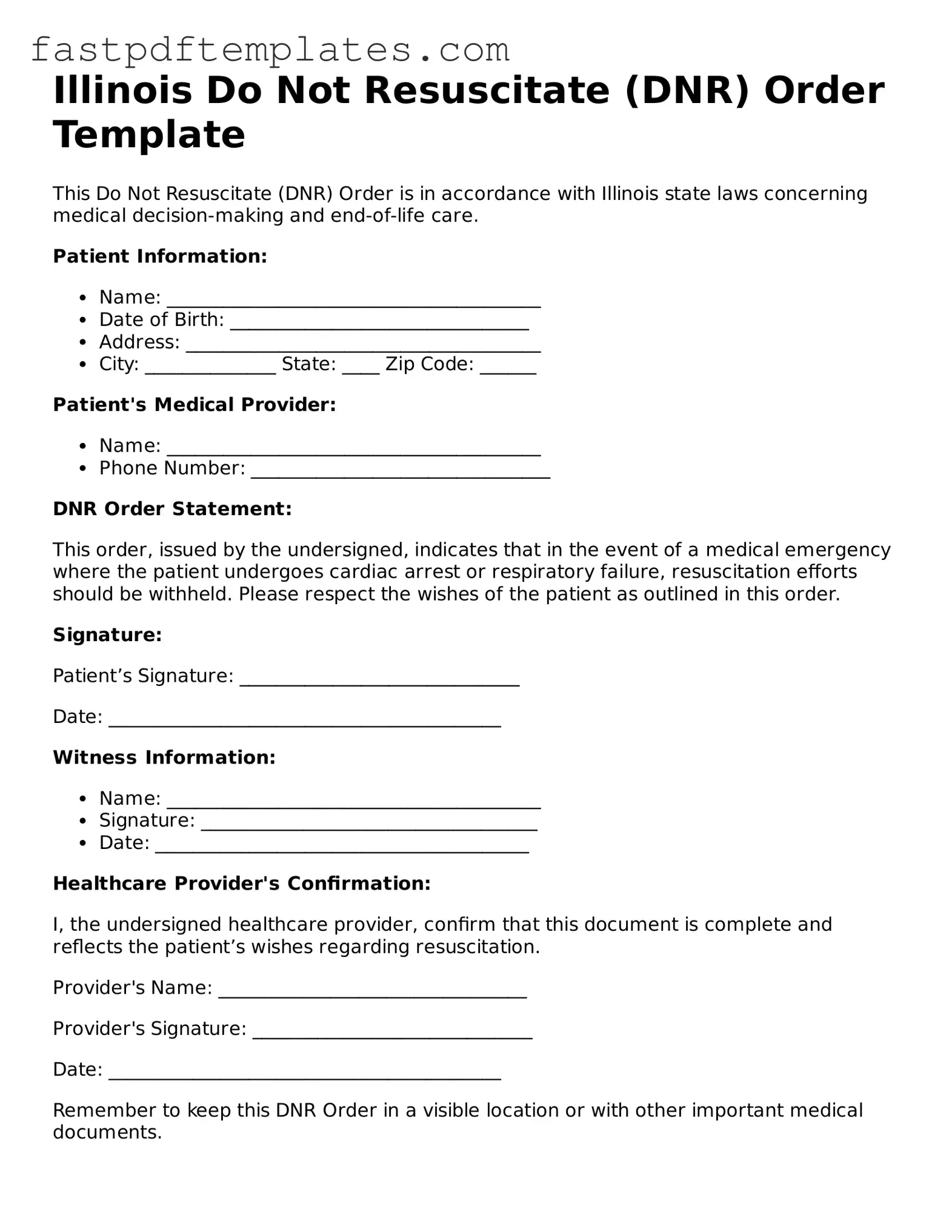
Attorney-Approved Illinois Do Not Resuscitate Order Document
Access Document
Your form still needs completion
Complete your Do Not Resuscitate Order online and download the final PDF.
Access Document
or
Click for PDF Form