Blank Cna Shower Sheets Form
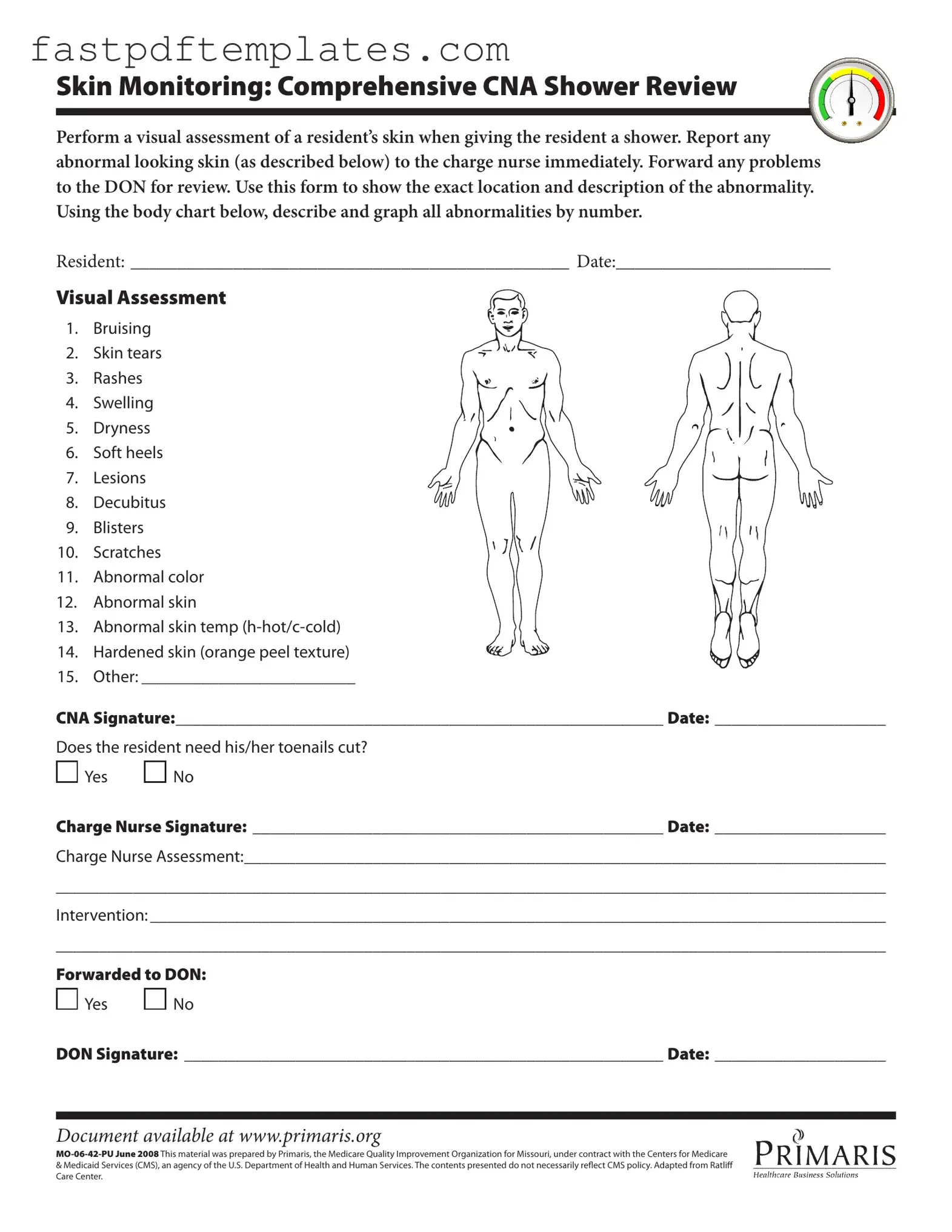
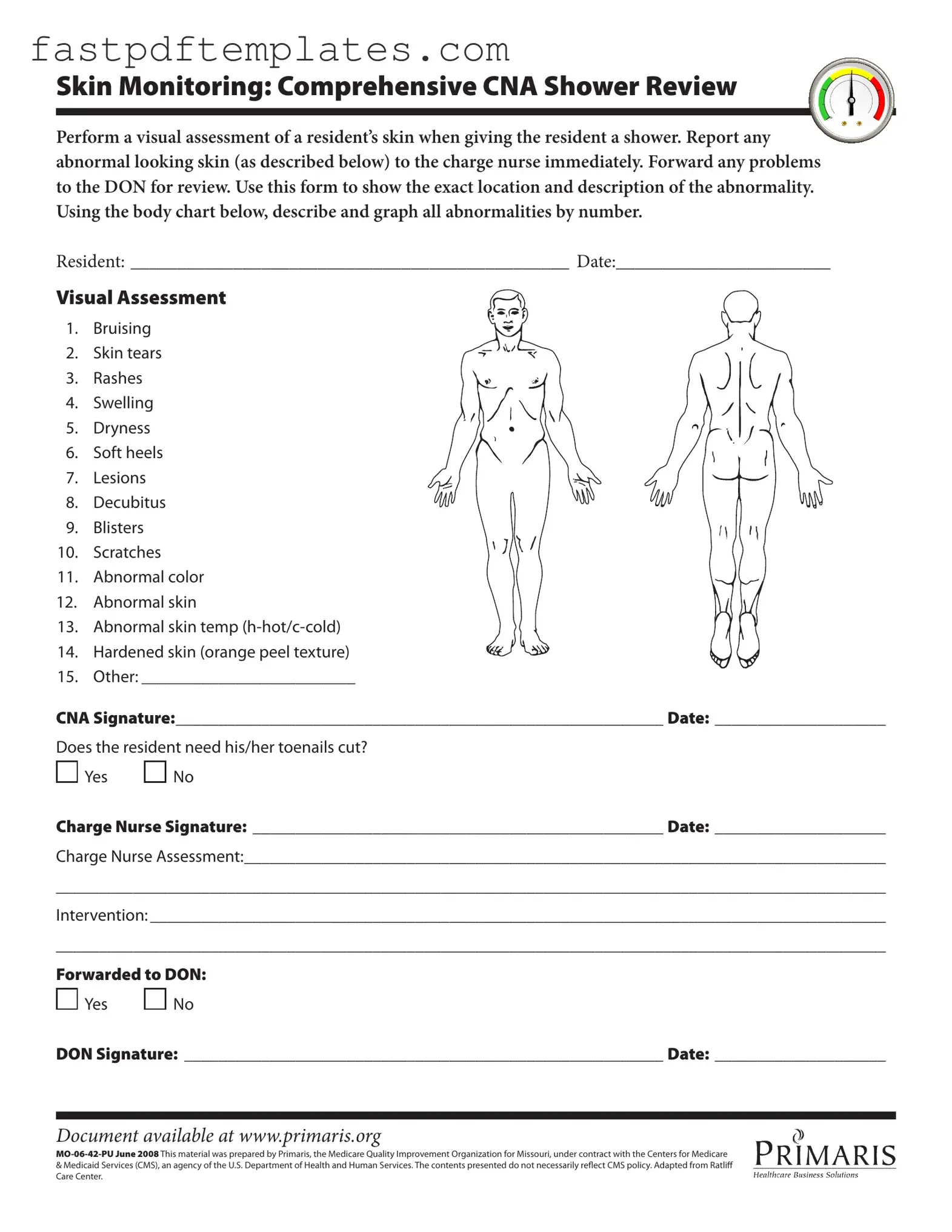
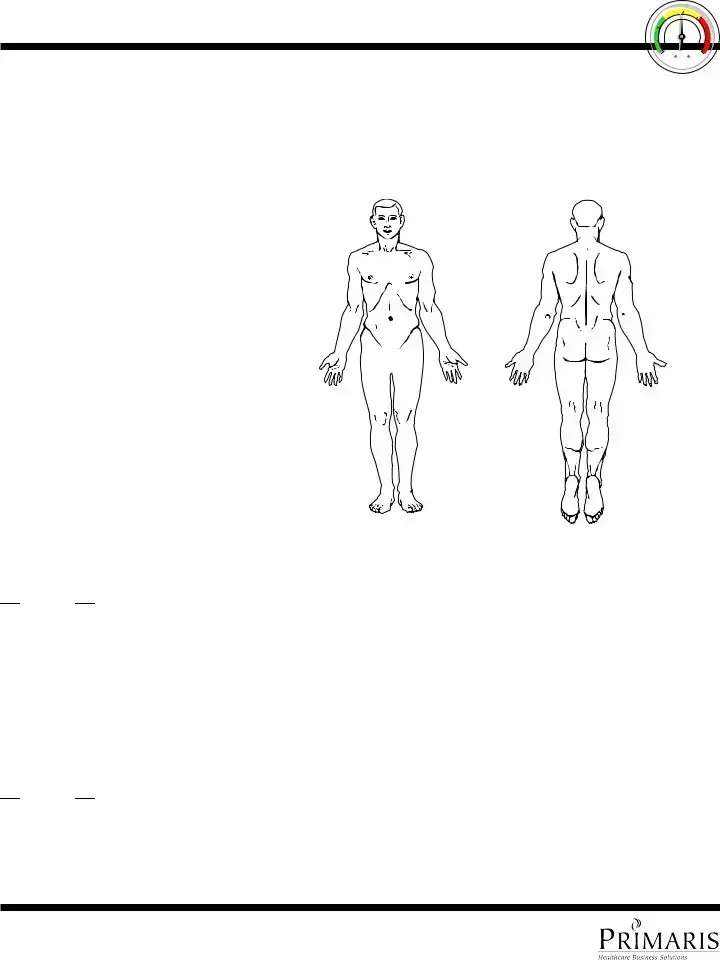
The CNA Shower Sheets form is a crucial tool used by certified nursing assistants to document the skin condition of residents during showering. This form facilitates a thorough visual assessment, enabling CNAs to report any abnormalities to the charge nurse promptly. By maintaining detailed records, the form supports effective communication and ensures that skin issues are addressed in a timely manner.
Access Document
Blank Cna Shower Sheets Form
Access Document
Your form still needs completion
Complete your Cna Shower Sheets online and download the final PDF.
Access Document
or
Click for PDF Form

 Yes
Yes 
 No
No
 Yes
Yes 
 No
No