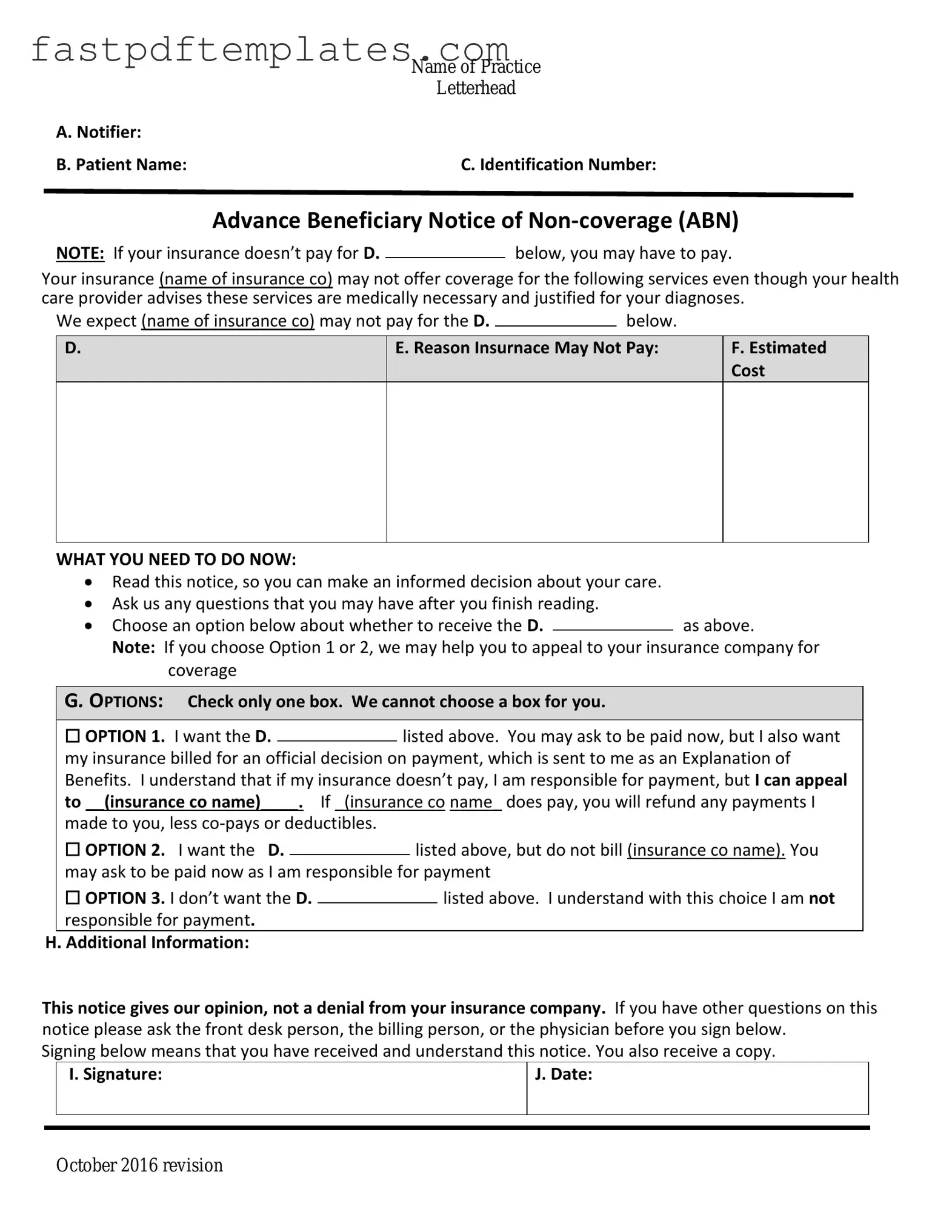
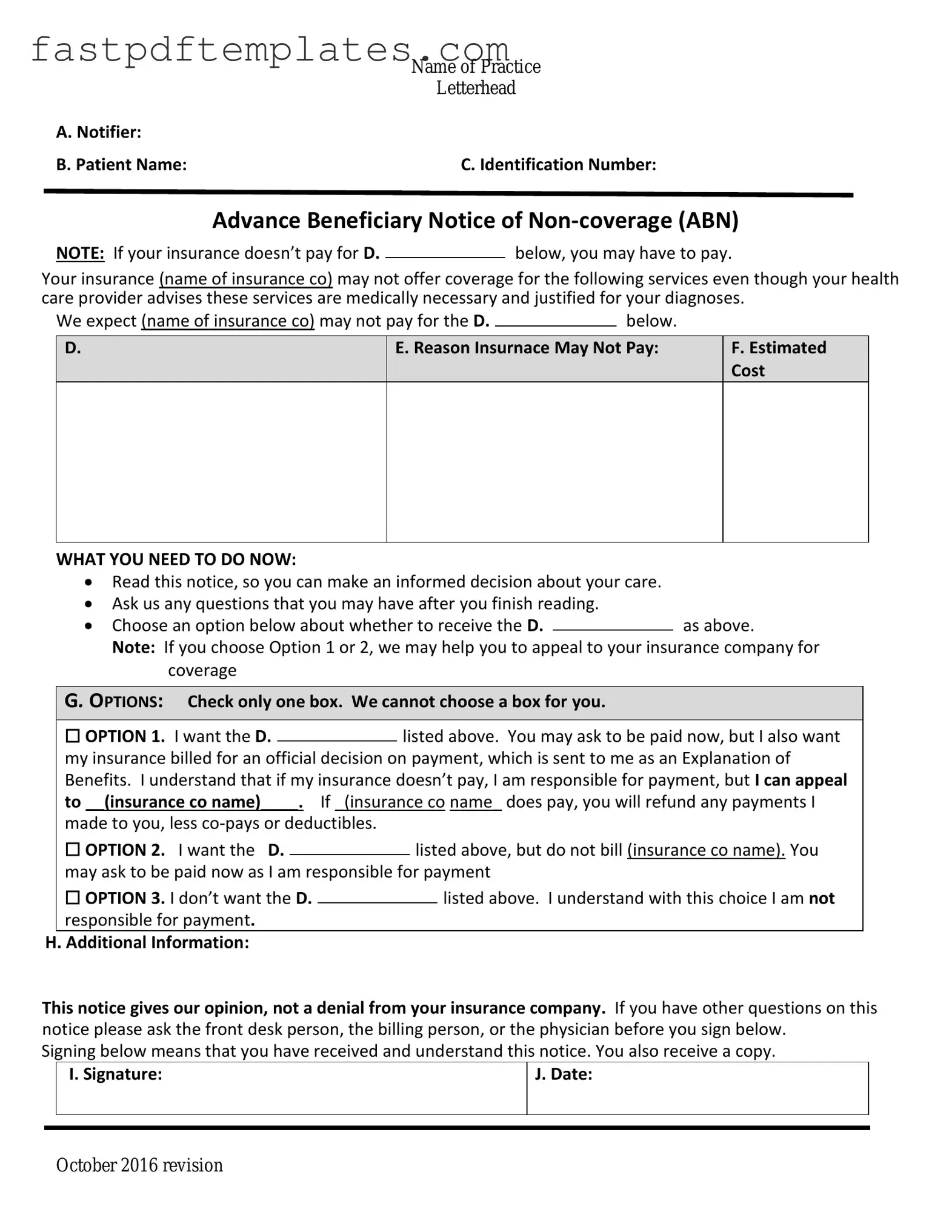
The Advance Beneficiary Notice of Non-coverage (ABN) form is similar to the Medicare Summary Notice (MSN). The MSN is a document that Medicare beneficiaries receive quarterly, summarizing the services received, costs, and whether Medicare paid for those services. Like the ABN, the MSN provides essential information regarding coverage decisions. Both documents aim to keep beneficiaries informed about their healthcare services and any potential costs they may incur if services are deemed non-covered by Medicare.
The Explanation of Benefits (EOB) is another document comparable to the ABN. Issued by private insurers, the EOB outlines the services provided, the amount billed, and the payment made by the insurer. Similar to the ABN, the EOB informs patients about their financial responsibility for medical services. Both documents serve as a means of communication between the healthcare provider, the insurer, and the patient regarding the coverage status of services rendered.
The Notice of Exclusion from Medicare Benefits (NEMB) also shares similarities with the ABN. This notice is issued when a service is not covered by Medicare, informing beneficiaries of their financial responsibility. Like the ABN, the NEMB helps patients understand why certain services may not be covered and what costs they might face. Both documents aim to clarify coverage issues and protect beneficiaries from unexpected bills.
The Out-of-Pocket Maximum Notice is another related document. This notice outlines the maximum amount a beneficiary may have to pay out-of-pocket for covered services in a given period. While the ABN informs patients about specific services that may not be covered, the Out-of-Pocket Maximum Notice provides a broader view of financial limits within a coverage year. Both documents enhance transparency in healthcare costs for patients.
The Pre-Authorization Request form is also similar to the ABN. This form is used when a healthcare provider seeks approval from an insurer before providing a service. Like the ABN, it helps ensure that patients are aware of potential coverage issues before receiving care. Both documents serve to mitigate the risk of unexpected costs for the patient by clarifying coverage requirements in advance.
Lastly, the Patient Financial Responsibility Agreement can be compared to the ABN. This agreement outlines the financial obligations of the patient for services rendered, especially when insurance coverage is uncertain. Similar to the ABN, it emphasizes the patient's responsibility for payment if services are not covered. Both documents aim to foster clear communication regarding financial expectations between healthcare providers and patients.